State of Oral Health Equity in America
To treat the whole person, our health system must better recognize the link between oral health and systemic health.

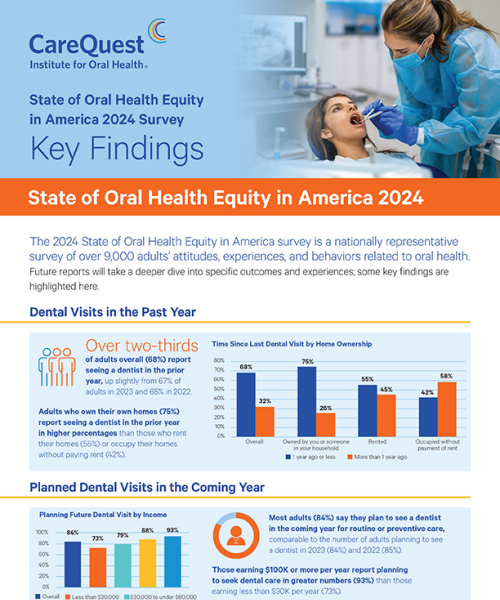
The State of Oral Health Equity in America is the largest nationally representative survey focused exclusively on adults’ knowledge, attitudes, experiences, and behaviors related to oral health.
The latest survey of more than 9,300 adults across the United States also collects information on how insurance coverage, oral health literacy, and access to a trusted provider can improve oral health opportunities and affect outcomes.
Findings from the survey allow oral health stakeholders to uncover and address oral health equity gaps.
Key Findings
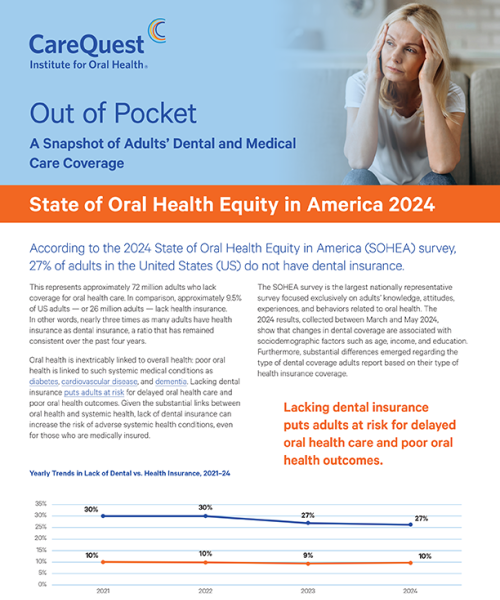
72M
Approximately 72 million adults in the US (27%) do not have dental insurance — almost 3 times the percentage of adults who lack health insurance.
Learn more
52%
More than half of Black adults (52%) have lost one or more teeth due to decay or gum disease, compared with 43% of all adults.
Learn more
1/4
One quarter of adults with a disability (25%) delayed care, missed an appointment, or were unable to obtain needed health care.
Learn more
$45B
Lost productivity time due to untreated dental disease costs the US an estimated $45 billion each year.
Learn more
2025 Reports
The Dental Home Is Where Good Oral Health Starts
Sociodemographic Factors Associated with Having a Usual Source of Dental Care
2024 Reports
Previous State of Oral Health Equity in America Reports
Methodology
The State of Oral Health Equity in America 2024 survey was designed by CareQuest Institute for Oral Health. Information was collected by NORC at the University of Chicago from March through May 2024, from adults 18 and older on the AmeriSpeak panel. AmeriSpeak is a probability-based panel designed to be representative of the US household population. Randomly selected US households were sampled using area probability and address-based sampling, with a known, non-zero probability of selection from the NORC National Sample Frame. Sampled households were contacted by US mail, telephone, and field interviewers. An additional general population sample was selected at the state level to increase the number of complete interviews for individual state oversamples. In 2024, a sampling unit of 22,448 was used, with a final sample size of 9,307 and a final weighted cumulative response rate of 41.5%. All data presented account for appropriate sample weights. The margin of error for the survey is 1.44%. All results presented are statistically significant at the p < 0.05 level unless otherwise noted.