Value-Based Care
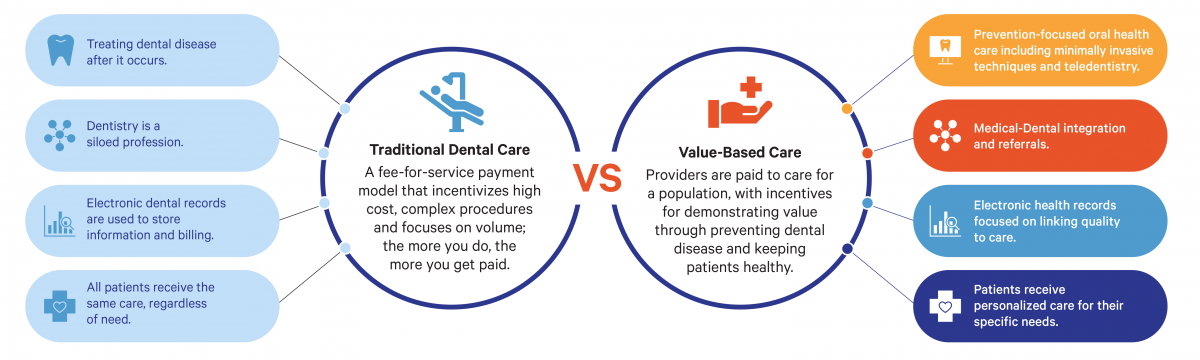
Shifting to value-based care — a system focused on quality over quantity — can lower costs and improve patient outcomes.
The Shift to Value-Based Care
In recent years, both medicine and dentistry have experienced a push to begin rewarding not the quantity of services but the quality of outcomes — a model known as value-based health care. This approach incentivizes prevention and personalization, and typically involves alternative payment models (APMs).
APMs can use different frameworks to:

Link financial incentives to improvements in care quality and health outcomes

Focus on disease management and prevention to lower spending

Pay for comprehensive and coordinated services
The advantages of a value-based care model are clear: less waste, lower costs, and, most importantly, better oral health for patients. Getting to that reality will take innovation, persistence, and a redesigned oral health care system. But the shift to value-based care is already showing promise.
The Benefits of Value-Based Care
Value-based approaches in dentistry focus on prevention and outcomes. They also involve integration of data, care across the continuum, and technological innovations such as teledentistry.
A successful value-based care model prevents dental disease and keeps patients healthy. And the payment model ensures a steady revenue stream even if there are fluctuations in care related to any disruptions to practice operations.
Improving the Patient Care Experience
For more than two centuries, dentists dentistry have has practiced in a fee-for-service (FFS) reimbursement environment. Workflow, care delivery, business plan, staffing, documentation, health information technology, scheduling, billing, goals, productivity, policies, procedures, and communication have all been designed and implemented around a care and financing model that emphasizes volume over value based on the quantity of services provided. The transition to value-based care (VBC) has the potential to change each of these areas in a significant way.
Signs of Progress
Federally Qualified Health Centers (FQHCs), which provide both medical and dental care, have been at the forefront of shifting toward an integrated model that includes value-based care. In Michigan, for example, MyCare Health Center, a participant in CareQuest Institute’s Community Oral Health Transformation (COrHT) initiative, decreased their cost per visit, decreased their no-show rates, and increased their net revenue within a system that provided quality care and yielded financial success.
COrHT, which also operated in North Carolina from 2022–2024, provided a framework for safety net dental clinics to help transform oral health care delivery so it is:
- Accessible to everyone through innovations ― like telehealth ― that provide care to people who have been traditionally underserved.
- Focused on prevention and minimally invasive care, including fluoride applications.
- Integrated with medical care to treat the whole person, because oral health and systemic health are connected.
Stats
51%
In a recent survey, half of (51%) of responding providers had never heard of APMs in dentistry, while 35% had only heard of APMs or knew a little about them, showing that building awareness will be critical in the coming years.
Learn more
635%
Teledentistry visits increased by 635% in participating North Carolina practices during COrHT, significantly expanding access to preventive care for underserved and rural populations.
Learn more
70%
APMs are increasingly being used both in Medicaid and Medicare. Nearly 70% of Medicaid beneficiaries are enrolled in managed care plans — plans focused on managing costs and patient utilization.
Learn more
The Path Ahead for Value-Based Care
Shifting to value-based care and APMs in dentistry involves a significant transformation. Education and outreach will play a critical role. In addition, we need further testing and piloting of value-based care models in dentistry. To make the shift, dental practices will need appropriate technology infrastructure, reporting and analytics systems, and methods to predict utilization and costs.