Enter your email to receive the CareQuest newsletter:
September 16, 2025
By Stacey Auger, MPH, Policy Consultant, CareQuest Institute
Federal leaders have made steep cuts to Medicaid in the recent budget and spending bill, but one thing remains clear: Medicaid matters.
And dental coverage matters — to individuals, families, local communities, and states.

Research consistently shows that dental coverage leads to greater access to — and utilization of — regular dental care. This, in turn, leads to improved health outcomes, lower overall health care costs, fewer emergency department visits, improved school outcomes, and greater workforce productivity.
Fortunately, many policymakers and state leaders continue to recognize the significance of adult dental benefits. As shown in our newly updated Medicaid Adult Dental Coverage Checker, there are key gains from 2024 and the first half of 2025:
- More states now offer extensive adult dental benefits.
- Several states meaningfully extended coverage for all adults.
- Increases in annual benefit maximums (ABMs) are helping to increase access to care.

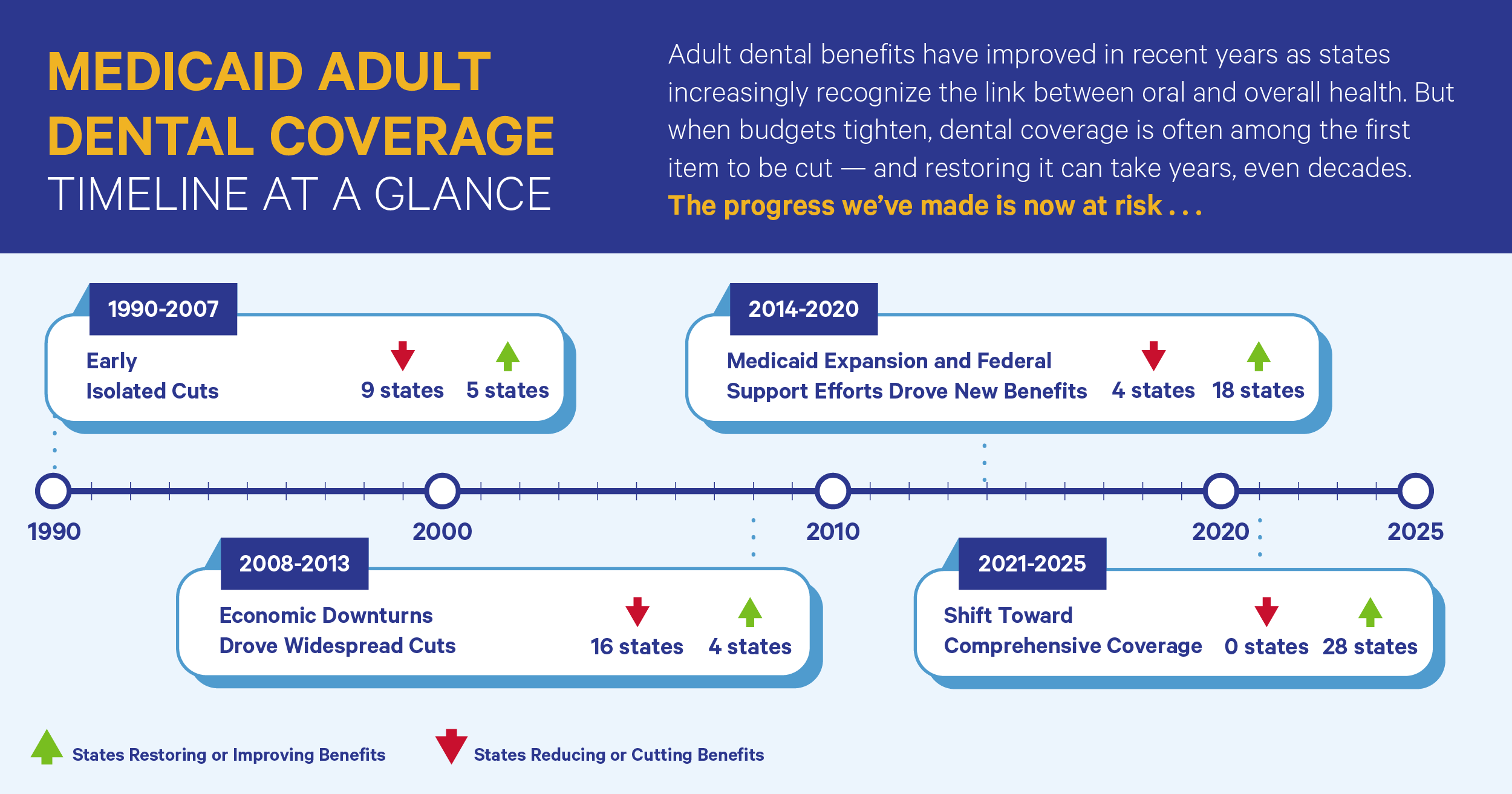
Yet these trends come at a time when Medicaid budgets are under significant threat. When state budgets are tight and cuts are needed, optional benefits are often the first to go. Between 2000 and 2025, at least 21 states reduced or eliminated benefits for some or all adult Medicaid beneficiaries. The results were devastating — beneficiaries went without necessary care, leading to pain, worsening health conditions, and increased use of hospital emergency departments — and, ultimately, drove up health care costs.
This year’s Coverage Checker shows both how far we’ve come and how much we have to lose. Below are this year’s most noteworthy takeaways.
1. The number of states with an extensive benefit continues to grow.
As of December 31, 2024, 11 states and DC meet the criteria for providing an extensive Medicaid adult dental benefit: Alaska, Iowa, Maine, Minnesota, Montana, Nebraska, New Jersey, Oregon, Tennessee, West Virginia, Wisconsin, and DC.
How do we know? Since 2020, CareQuest Institute for Oral Health, ADA Health Policy Institute, the Center for Health Care Strategies, Inc., and an advisory committee of state and national leaders have conducted an annual survey of state Medicaid agencies.
In order to meet the survey’s criteria for an extensive Medicaid adult dental benefit, a state must have an ABM of $1,000 or greater and provide coverage of specific CDT codes within seven dental service categories: diagnostic (exams), preventive (cleanings and fluoride treatments), restorative (fillings and crowns), endodontic (root canal therapy), periodontal (scaling and root planing and periodontal maintenance), prosthodontic (dentures, relines, and rebases), and extraction services. Coverage must be offered to all adult beneficiaries.
Based on this survey, and as displayed in the Coverage Checker, we can see that the number of states that provide an extensive benefit to all their adult beneficiaries has increased every year since 2020. In our first year of surveying, four states met the criteria. The number increased to seven in 2022 and nine in 2023.
The graphic below illustrates how states have strengthened — and cut — adult dental benefits in the past 35 years. Gains from the past decade, in particular, are now at risk.
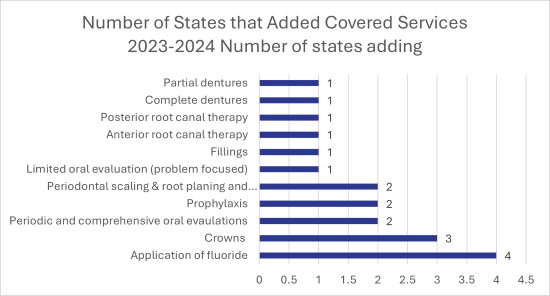
2. New and meaningful expansions of covered services went into effect in the last year.
In 2024, nine states broadened their benefit offerings by one or more services (e.g., cleanings, periodontal services, partial dentures) and/or increased the frequency of existing services (e.g., increasing coverage of cleanings from once to twice per year).
The most commonly added services were preventive services: cleanings and application of fluoride.
Two states (Georgia and Kansas) began providing coverage of cleanings and four states (Georgia, Kansas, Minnesota, and West Virginia) began providing coverage for the application of fluoride. It is important to note that in Kansas prior to 2024, these services were provided as “value-added benefits” (VABs) by the state’s Medicaid-contracted managed care organizations.
Georgia, Kansas, and Minnesota saw the greatest expansions of benefits overall from 2023 to 2024.
- Georgia: Thanks to an $11 million increase in the FY 2025 budget, Georgia’s Medicaid dental program expanded coverage in 2024. Effective July 1, 2024, coverage of oral evaluations, cleanings, application of fluoride, fillings and crowns, anterior and posterior root canal therapy, and complete and partial dentures is available to all adult beneficiaries . Prior to this benefit expansion, the majority of adult beneficiaries were covered only for limited oral evaluations and emergency extractions.
- Kansas: In the spring of 2024, the Kansas Legislature approved additional funding to cover examinations and cleanings — services that have been offered by the state’s three Medicaid-contracted managed care organizations as “VABs” since 2013. How the VABs were structured varied by managed care organization and from year to year, thus making the system difficult to navigate. Making these preventive services part of the state Medicaid dental benefit allows for more predictability to consumers and providers and is expected to increase adult access to dental care.
Minnesota: In May 2023, state lawmakers signed the Health and Human Services omnibus bill into law. Among other provisions, this legislation required the state to provide dental benefits based on medical necessity to all Medicaid-enrolled adults, regardless of age or pregnancy status. This change took effect January 1, 2024. In 2009, Medicaid dental benefits for adults were significantly reduced due to budget cuts. In the years following, Minnesota had two different dental benefit sets for Medicaid enrollees, including a benefit set for pregnant adults and children and a benefit set for nonpregnant adults. While pregnant adults and children under the age of 21 received extensive benefits, many adult enrollees were not covered for these same services until this year.
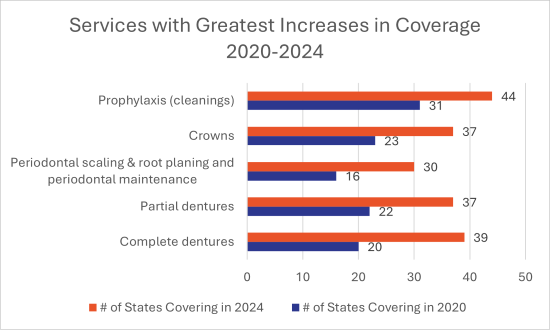
3. Increases in coverage have taken place in every service category since 2020.
There have been significant increases in coverage across all seven service categories since our first round of surveying in 2020. The services with the biggest gains are cleanings, complete and partial dentures, periodontal scaling and root planing and periodontal maintenance, and crowns.
4. States are making changes to their ABMs to increase access to needed services.
Another area of positive change is in ABMs, or the annual limit states place on dental service spending per member per year.
ABMs are generally put in place by states to control annual program costs. In some instances, they can limit individual patient access to care because treatment needs may exceed the annual limit. In such instances, a patient may need to delay care or forego it entirely.
In 2020, six states had an ABM of less than $1,000, six had an ABM of $1,000 or greater, and 32 states placed no limit on dental service spending per member.
In 2024, by comparison, one state had an ABM of less than $1,000, 14 had an ABM of $1,000 or greater, and 35 states placed no limit on dental service spending per member. In 2024, Nebraska and West Virginia lifted their ABM. Each cited the limiting effect on access to care their previous ABM had for beneficiaries.
Nebraska first implemented an ABM of $1,000 in 2008. It then reduced the ABM to $750 in 2021. In lifting the ABM in January 2024, the Nebraska Department of Health and Human Services noted that the $750 ABM “creates a barrier to care for new and high-need members who may need additional dental care. Removing the dental benefit maximum will improve member access to care and remove an administrative obstacle for dentists across the state.”
West Virginia implemented a $1,000 ABM in 2021 when the state extended its Medicaid adult dental benefits. In July 2024, the state increased its ABM to $2,000. This limit applies to all covered diagnostic, preventive, and restorative procedures, and was implemented with the express purpose of allowing beneficiaries to obtain a full set of dentures at the same time.
5. States continue to recognize the enhanced needs of certain populations.
Recognizing the distinct oral health needs of certain groups of adult beneficiaries, some states have opted to provide additional or enhanced services to these groups — most notably pregnant and postpartum adults, those with certain health conditions, adults with intellectual and/or developmental disabilities, and those utilizing long-term care.
In 2024, 21 states reported that they offer different coverage to specific groups of beneficiaries than they offer to other adult beneficiaries ages 21–64.
Two states, Connecticut and Utah, added coverage for certain groups in 2024.
Historically, Connecticut has not covered periodontal services for its adult members. Effective January 1, 2024, Connecticut Medicaid began covering periodontal services for certain adult beneficiaries. To be eligible, members must have treatable periodontal disease and be diagnosed with certain chronic health conditions.
Utah eliminated non-emergency dental services for all but pregnant adults in 2009. Beginning in 2017, and in partnership with the University of Utah School of Dentistry, the state began providing adult dental benefits incrementally by population group (seniors, adults with disabilities, adults enrolled in the state’s Targeted Adult Medicaid program). Effective January 1, 2024, Utah Medicaid and the Children’s Health Insurance Program (CHIP) extended dental coverage for pregnant members from 60 days to 12 months postpartum.
CareQuest Institute’s report on coverage offered to specific beneficiary groups, updated in 2025, outlines what adult dental benefits are available through each state’s Medicaid program.
6. Benefits are constantly evolving.
Although our survey captures coverage updates through December 31, 2024, changes at the state level happen throughout the year. In the first six months of 2025 alone, several states took very promising steps to improve coverage and access to care.
- Utah: After years of extending Medicaid adult dental benefits incrementally by population group, Utah began offering dental benefits to all adults effective April 1, 2025.
This change was initiated in 2023 when the Utah legislature passed Senate Bill 19, which directed the state to pursue federal Medicaid waivers to extend Medicaid dental care to all adults 21 years of age and older. Utah’s 1115 Waiver was approved on January 8, 2025, and expanded dental benefits took effect April 1, 2025. All adult beneficiaries are now covered for exams, X-rays, cleanings, fillings, crowns, root canals, dentures, and extractions.
- Nevada: In 2019, the Nevada legislature passed AB223, which directed the state to pursue federal Medicaid waivers to expand Medicaid dental benefits to nonpregnant adults diagnosed with diabetes. Approved on July 19, 2024, the 1115 Waiver will allow beneficiaries to receive a limited dental benefit package, including diagnostic and preventive, restorative, endodontic, and periodontic dental services through the provider network of selected Federally Qualified Health Centers (FQHCs) and participating Tribal Health Centers with dental clinics. The new benefits are expected to take effect by the end of this year.
As noted in the approval letter, “This demonstration furthers the objectives of Medicaid by improving access to dental services in Nevada for certain Medicaid-enrolled adults. Through these efforts, the state will be able to test the value of improved access to oral health care on enrollee health outcomes and in controlling expenditures for a high-risk adult diabetic population in Medicaid. Nevada does not currently cover non-emergency dental benefits for its non-pregnant adult or parent population; this demonstration is a helpful tool to test the potential return on investment of providing dental benefits for this population.”
- Arkansas: State legislators signed a new bill into law in April 2025 to increase the ABM for adults with special needs. The ABM was increased from $500 to $1,000 and is expected to take effect in September 2025.
Additionally, the legislation increases reimbursement rates for oral and maxillofacial surgeons’ dental services, pediatric dental services, and dental services for adults with special needs.
- Virginia: Since 2015, Virginia has provided comprehensive Medicaid adult dental benefits to pregnant beneficiaries. In 2021, this coverage was extended from two months to 12 months postpartum. Lawmakers signed a bill into law in March 2025 that codifies the dental benefits provided to pregnant and postpartum beneficiaries.
The bill — one of several this session aimed at improving maternal and child health outcomes — specifies that pregnant beneficiaries will be eligible for at least four dental visits during their pregnancy, with the possibility of additional visits recommended by a licensed dentist or obstetrician. Additionally, and for the first time since extending benefits to pregnant beneficiaries, the bill requires the Department of Medical Assistance Services to submit an annual report to the governor and General Assembly detailing the implementation of these dental services, including the number of pregnant women who used the services, the impact on maternal and infant health outcomes, any access barriers, and recommendations for future improvements. The first such report is to be submitted by November 1, 2026, providing an opportunity to evaluate the effectiveness of the expanded dental care coverage for pregnant beneficiaries.