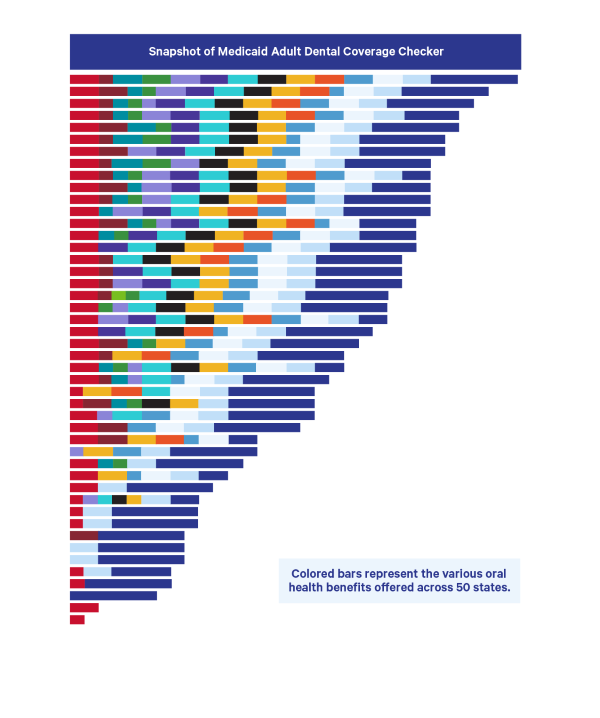
 This week, CareQuest Institute for Oral Health released the Medicaid Adult Dental Coverage Checker in partnership with the American Dental Association (ADA) Health Policy Institute, the Center for Health Care Strategies, Inc., and the National Academy for State Health Policy. The Checker provides a snapshot of a state’s Medicaid adult dental benefits, allowing individuals to better understand the details of their state’s offerings and identify potential areas for improvement. (It’s important to note that the Checker contains information on benefits in the spring of 2020; several states have expanded in the last two years.)
This week, CareQuest Institute for Oral Health released the Medicaid Adult Dental Coverage Checker in partnership with the American Dental Association (ADA) Health Policy Institute, the Center for Health Care Strategies, Inc., and the National Academy for State Health Policy. The Checker provides a snapshot of a state’s Medicaid adult dental benefits, allowing individuals to better understand the details of their state’s offerings and identify potential areas for improvement. (It’s important to note that the Checker contains information on benefits in the spring of 2020; several states have expanded in the last two years.)
For many years, policymakers and advocates have relied on the ADA classification system to see these benefits. Adopted and adapted by other organizations, this system classifies Medicaid adult dental benefits into four categories: extensive, limited, emergency, and none. While this classification system has served the oral health community well for many years, the four organizations decided that states would benefit from a classification system that provides clear guidance on:
- the specific covered service categories necessary to constitute an extensive benefit
- the specific procedures to be covered within each service category
- the specific service frequency to be covered
- whether coverage is offered to all adult Medicaid beneficiaries or only to select subsets
Michael Monopoli, DMD, MPH, MS, FACD, FICD, vice president of grant strategy at CareQuest Institute, and Stacey Auger, MPH, a policy consultant at CareQuest Institute, have been at the center of the core team that has worked on this project for the last several years. Below, they share more about the origins and goals of the Coverage Checker.
Let’s start at the beginning. What was the impetus to develop a new way to look at Medicaid adult dental benefits?
Mike and Stacey: The idea came to us during the Oral Health 2020 Campaign after a period of very significant expansion and restoration of Medicaid adult dental benefits in several states. CareQuest Institute and the ADA Health Policy Institute collaborated to update the ADA’s classification of states based on these policy wins. After doing so, we shared the new round of state classifications with our grantees and partners, which led to a robust discussion regarding benefit levels and state placement within the classification system.
CareQuest Institute convened a workgroup that quickly decided the oral health community would benefit from a new assessment tool. We wanted to develop something that moved us beyond simply counting the number of procedures covered.
Why is it important for oral health stakeholders to understand the details of adult dental benefits?
Mike and Stacey: As we learn more about the connections between oral health and overall health, we need to strengthen state programs and services to ensure they’re improving oral health and meeting patient needs. A dental benefits package that includes coverage for a robust array of services — diagnostic, preventive, restorative, endodontic, periodontal, prosthodontic, and extractions — has the best chance of doing that.
States need to understand what constitutes an extensive benefit, and the Coverage Checker can help. It not only defines what an extensive benefit is, but it also outlines the specific covered service categories necessary to constitute an extensive benefit, the specific procedures to be covered within each service category, and the specific service frequency to be covered.
We’d like to see all states offer an extensive benefit to all their Medicaid adult beneficiaries. But we also know that improving benefit packages can take time and that some states will need to take an incremental approach.
Can you talk about the Rubric that yielded the data for the Medicaid Coverage Checker? How was it created?
Mike and Stacey: The Rubric is a survey designed to be completed by state dental directors or their equivalents. It defines an extensive Medicaid adult dental benefit and assesses the extensiveness of existing coverage within each state. This is done by looking at coverage of specific procedures and services, including allowed frequency, in eight service categories. The categories of procedures encompass specific services that are most commonly reimbursed by employer-based dental benefit plans and that are critical to maintaining lifelong oral health.
Being part of the development process of the Rubric and Coverage Checker was an incredible experience! Our Core and Advisory Group members drove this process. Together, we worked with a wide range of subject matter experts and leaders at national, state, and local levels throughout every stage. For a few years, we solicited input and guidance from these leaders and experts. We also engaged in multiple rounds of review and revision to the definition and the survey tool, and conducted two full rounds of beta testing.
The survey was formally released to all state Medicaid dental directors or their equivalents in the 50 states and DC in the spring of 2020. This was done in partnership with the Medicaid|Medicare|CHIP Services Dental Association (MSDA) and in conjunction with their National Profile of State Medicaid and CHIP Oral Health Programs.
We were thrilled to secure responses from all 50 states and DC — no small feat to have accomplished as states were stretched, strained, and in the throes of the pandemic response. (Sidenote: Thanks to all the directors who made time for this!)
State dental directors had to buy into this process. How did you accomplish that?
Mike and Stacey: The development of the Rubric and Coverage Checker involved a wide array of stakeholders, including state dental directors. Directors were engaged throughout the entire process and were actively involved in reviewing, revising, and beta testing the Rubric. Specifically:
- Our Advisory Group includes a current state dental director (Donna Balaski, DMD) and a former state dental program consultant (Robert Isman, DDS, MPH).
- Dental directors (or their equivalents) in more than half the states participated in one or both rounds of beta testing and provided feedback on the content and usability of the Rubric.
- Staff and an advisory committee of MSDA provided a full technical review of the Rubric.
- Members of the Core Group presented the Rubric at the 2020 MSDA National Symposium.
- Members of the Core Group shared the 2020 data with state dental directors at an MSDA “Coffee Hour” in the spring of 2021. As a result of that meeting, we removed two questions from the survey.
- Members of the Core Group shared revised results and a preview of the Coverage Checker with a cohort of 10 state dental directors in the spring of 2022. We made several structural changes to the Coverage Checker based on that feedback.
Is there an intended audience for the Medicaid Coverage Checker? Who do you envision using this?
Mike and Stacey: The Coverage Checker was designed for a wide range of audiences:
- Medicaid agencies: It allows administrators to view the extensiveness of benefits offered in their state and in relation to others, and to determine what improvements are needed to achieve a more extensive benefit.
- Advocates: It allows local and state advocates to better understand the coverage landscape in their state and others, and to support efforts to implement/restore benefits.
- Legislators and other policymakers: It provides leaders with a definition of an extensive dental benefit and an understanding of the benefits offered in their state on a continuum from no benefits to extensive.
How will the Medicaid Coverage Checker move the needle on improving the oral health of all?
Mike and Stacey: We are learning more every day about the critical role oral health plays in overall health. Without regular care, oral health problems can develop and worsen, leading to overall health and social issues that can harm individuals.
Research shows that access to extensive dental benefits plays a crucial role in increasing access to — and utilization of — preventive care and reducing disparities in dental care visits, preventive services, and treatment services. We also know that providing dental coverage to adults increases the likelihood that their children will receive timely and appropriate care. Furthermore, adults with dental coverage are more likely to enter and remain in the workforce.
The Coverage Checker allows states to see where their benefits package falls on a continuum from no benefits up to extensive. In doing so, it allows them to identify areas for improvement and expansion.
Coverage of dentures is a great example of this. Many states cover full dentures, ranging from once every seven years to once per patient’s lifetime. Yet the average denture begins to wear out and should be evaluated for replacement within three to five years. The Rubric acknowledges this need and assesses coverage based on these timeframes.
This has been a long journey to get to the release of this tool. What’s next? Do you have plans to update it?
Mike and Stacey: Our first order of business is to make sure everyone knows about this new tool and how to use it. We’ll be doing a formal launch soon, which will include presentations, a webinar, and sharing information on partner websites. We’ll also be soliciting feedback and input on what additional resources stakeholders need and want.
We will then turn our attention to the next round of surveying. One of the main goals of the Rubric and Coverage Checker is to track movement in benefit offerings over time. We intend to conduct the Rubric survey on a regular basis and display results in the Coverage Checker.
What should people do if they have questions or feedback about the Medicaid Coverage Checker?
Mike and Stacey: We encourage questions and feedback and would love to hear from you!
